Keynote Addresses
Delivering keynote addresses at the Investing in Japanese Regenerative Medicine symposium were two distinguished speakers: Japan’s minister of health, labor and welfare Keizo Takemi and Norimasa Nakamura, a professor at Osaka Health Science University’s Institute for Medical Science in Sports and a guest professor at Osaka University’s Global Center for Medical Engineering and Informatics.
Building a Global Ecosystem for Drug Discovery

Keizo Takemi
Minister of Health, Labor and Welfare
Takemi delivered his remarks under the title, “The Current State and Future Prospects of Advanced Regenerative Medicine in Japan: Towards the Construction of a Global Drug Discovery Ecosystem.” He addressed that subject in the context of issues and objectives detailed in a position paper released by his ministry on Aug. 30, 2024, as “Near-Future Health Care Eco-System Strategy.”
The Ministry of Health, Labor and Welfare’s position paper notes the challenges posed by Japan’s declining birthrate, its shrinking and aging population, and digitalization and globalization. It notes, too, the need for ensuring a satisfactory quality of life for citizens who can increasingly live for close to a century or even more, while maintaining the viability of Japan’s universal health insurance. The strategic objectives highlighted in the paper include drawing on cutting-edge technologies to address those challenges. Especially prominent among the technologies cited in the paper and by Takemi in his talk is regenerative medicine.
A central plank in the health ministry’s near-term strategy is building a global ecosystem for drug discovery. Takemi emphasized the global stance evoked in that plank and stressed that it represents a fundamental change in orientation for his ministry. “The ministry has been,” he acknowledged, “very domestically oriented. But that has changed. We will now bring both an internal perspective and external perspective to issues.”
Building a global drug discovery ecosystem will include fortifying Japan’s drug discovery clusters with incubation and accelerator functions for startups. It will also include tapping private-sector resources to help shepherd academic discoveries toward commercialization, starting at the preclinical stage. A framework outlined by Takemi will speed the progress of universities’ drug discovery “seeds” through proof of concept and into first-in-human clinical trials.
Takemi introduced joint work by Keio University and the Murayama Medical Center, a national hospital in Tokyo, in treating spinal cord injuries with regenerative medicine. They use neural progenitor cells derived from induced pluripotent stem (iPS) cells provided by Kyoto University. Physicians at Keio University inject the neural progenitor cells into patients’ spinal cord lesions, and the patients then undergo a year of rehabilitation and observation at the Murayama Medical Center.
A 2024 revision of Japan’s Act on the Safety of Regenerative Medicine brought in vivo gene therapy under the scope of the act. That was part of continuing efforts, explained Takemi, “to safely promote emerging technologies. Moving forward, we will continue to create an environment that enables the safe provision of regenerative medicine and will work to promote innovation in this field.”
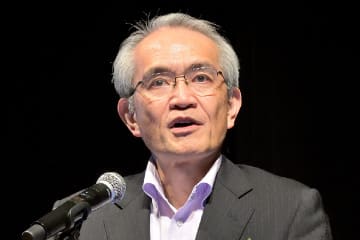
Applying Regenerative Therapy to Joint Disease

Norimasa Nakamura
Professor, Osaka Health Science University’s Institute for Medical Science in Sports
Guest Professor, Global Center for Medical Engineering and Informatics, Osaka University
Nakamura spoke on the status of the clinical application of regenerative therapy to joint disease in Japan. “The human body,” he began, “has more than 260 joints. Between the bones at the joints is cartilage, which performs load distribution, shock absorption, and lubrication. Cartilage contains no blood vessels and is therefore unable to repair itself. If the cartilage suffers damage, the damaged area will expand over time. That can lead to damage to the bones and to osteoarthritis.”
Osteoarthritis will afflict more than 20 million Japanese by 2040, according to Nakamura’s interpolation from a projection by the U.S. Centers for Disease Control and Prevention. He also cited troubling statistics from Japan’s Ministry of Health, Labor and Welfare about life expectancy overall and healthy life expectancy. According to those statistics, average life expectancy at birth was 87.4 years for Japanese women and 81.4 years for Japanese men in 2019, but the average expected span of life unlimited by significant health problems was only 75.4 years for women 72.7 years for men. “Our mission,” Nakamura declared, “is to help people live active lives throughout their lifespans.”
Japan’s health ministry reports that osteoarthritis accounts for 11% of the disorders responsible for the gap between overall lifespan and healthy lifespan and that bone fractures, a lot of which are attributable to osteoarthritis, account for 13%. “So preventing and alleviating osteoarthritis is especially important,” stressed Nakamura, “in ensuring the quality of life.”
Nakamura acknowledged that artificial joints are an option when cartilage has deteriorated, but he cautioned that they entail a loss of flexibility and that saving joints would be preferable to replacing them, if possible. He discussed three techniques that offer promise for saving joints.
One joint-saving technique discussed by Nakamura was autologous chondrocyte implantation. Chondrocytes, the only cells in cartilage, produce and maintain the cartilaginous matrix. “Autologous” means removing cells from a patient, culturing them outside the body, and injecting them back into the patient — into an afflicted joint in the case of chondrocytes. Nakamura shared a 2014 paper by U.S. researchers that reported success with this technique in 137 patients.
The two other joint-saving techniques discussed by Nakamura use iPS cells (embryonic stem cells) and mesenchymal stem cells (adult stem cells). Mesenchymal stem cells can differentiate into any of a limited range of tissue types, including cartilage, bone, and muscle, and iPS cells can differentiate into any kind of tissue. Nakamura described in great detail several initiatives in Japan and in the United States for using mesenchymal stem cells to repair damaged cartilage. He was especially emphatic about recent verification that mesenchymal stem cells disappear after they perform their work and that they therefore pose no risk of triggering the body’s rejection mechanism.
HOME
Investing in Japanese Regenerative Medicine

PAGE 1
Keynote Addresses

PAGE 2
Authoritative Perspectives on Governing and Nurturing Regenerative Medicine

PAGE 3
Prominent Japanese Venture Companies in Regenerative Medicine and Drug Discovery

PAGE 4
Entrepreneurship and Venture Capital
PAGE 5